Intra-Aortic Balloon Pump (IABP)⁚ An Overview
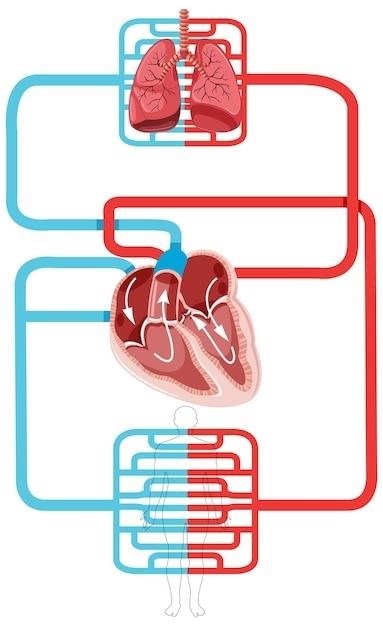
The intra-aortic balloon pump (IABP) is a temporary circulatory support device that augments cardiac output and improves myocardial perfusion. It involves a balloon catheter inserted into the aorta, inflating during diastole and deflating during systole to enhance coronary blood flow and reduce afterload. IABP is used to treat various conditions, including cardiogenic shock and acute myocardial infarction, often as a bridge to other therapies.
IABP Mechanism and Hemodynamic Effects
The IABP functions through synchronized counterpulsation. A balloon catheter, positioned in the descending aorta, inflates during diastole (ventricular relaxation), augmenting diastolic aortic pressure and increasing coronary artery perfusion. This enhanced blood flow delivers more oxygen to the myocardium. Simultaneously, the balloon deflates just before systole (ventricular contraction), reducing afterload on the left ventricle. This decreased resistance allows for easier ejection of blood, improving cardiac output. The net effect is increased myocardial oxygen supply and reduced myocardial oxygen demand. Precise timing of inflation and deflation is crucial for optimal hemodynamic benefits. The IABP’s effectiveness depends on factors like balloon size, inflation/deflation timing, and patient-specific hemodynamic characteristics. Incorrect timing can reduce efficacy or even be detrimental. Monitoring of hemodynamic parameters is essential to assess the IABP’s impact and to adjust therapy as needed. The system’s performance is also influenced by the patient’s aortic compliance and systemic vascular resistance. Monitoring and adjusting therapy are vital to maximize positive effects and minimize potential complications.
Indications for IABP Use
IABP is indicated for patients experiencing critical hemodynamic instability where temporary circulatory support is needed. Key situations include cardiogenic shock following acute myocardial infarction (AMI), where the heart is unable to pump sufficient blood. It’s also used for patients undergoing high-risk percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) surgery, particularly those with severely impaired left ventricular function. IABP can serve as a bridge to coronary revascularization, allowing time for myocardial recovery or preparation for more definitive interventions. It might be employed in cases of acute mitral regurgitation, where severe valve leakage compromises cardiac output. Other potential uses include unstable angina refractory to medical management, and post-operative cardiac failure following cardiac surgery. The decision to use IABP is made on a case-by-case basis, considering the patient’s overall clinical status, hemodynamic profile, and the potential benefits versus risks. Careful assessment is crucial to ensure appropriate patient selection.
IABP Procedure and Catheter Insertion
IABP insertion is typically performed in a cardiac catheterization laboratory or intensive care unit by experienced cardiologists or interventionalists. After appropriate anesthesia and anticoagulation, a femoral artery access is commonly used, although other approaches such as axillary access may be considered. Under fluoroscopic guidance, a sheath is inserted into the artery, followed by the IABP catheter. The balloon catheter is advanced into the descending thoracic aorta, its position confirmed fluoroscopically to ensure optimal placement for counterpulsation. Accurate positioning is crucial for effective hemodynamic support. Once correctly positioned, the balloon is connected to the IABP console, which controls inflation and deflation timing synchronized with the electrocardiogram (ECG). The system is then activated and hemodynamic parameters are continuously monitored to assess the effectiveness of the therapy. Post-insertion, careful monitoring of the insertion site and the patient’s overall hemodynamic status is essential to detect potential complications.
IABP⁚ Clinical Applications and Outcomes
IABP improves hemodynamics in various clinical scenarios, including cardiogenic shock and acute myocardial infarction. It serves as a bridge to definitive therapies like coronary artery bypass grafting (CABG) or percutaneous coronary intervention (PCI), ultimately aiming to enhance patient survival and recovery.
IABP in Cardiogenic Shock and Acute Myocardial Infarction
In cardiogenic shock, a life-threatening condition where the heart fails to pump enough blood, IABP plays a crucial role in stabilizing the patient. By augmenting coronary perfusion pressure and reducing afterload, it improves myocardial oxygen supply and demand balance. This is particularly beneficial in the context of acute myocardial infarction (AMI), where a significant portion of the heart muscle is compromised. The IABP helps to maintain adequate blood pressure and organ perfusion while allowing time for revascularization procedures such as PCI or CABG. Studies have shown that IABP can improve survival rates and reduce the need for more invasive interventions in selected patients with AMI complicated by cardiogenic shock. However, the optimal timing and patient selection remain areas of ongoing research and debate. The decision to use IABP is made on a case-by-case basis, considering the patient’s overall clinical picture and hemodynamic profile.
IABP as a Bridge to Other Therapies
Often, IABP serves as a temporary measure to stabilize critically ill patients before more definitive treatments can be implemented. It buys valuable time for interventions such as coronary artery bypass grafting (CABG), percutaneous coronary intervention (PCI), or the implantation of a left ventricular assist device (LVAD). By improving hemodynamics and myocardial perfusion, IABP reduces the risk of complications during these procedures. The temporary support provided by IABP allows the heart to recover, reducing the severity of the underlying condition and improving the chances of successful long-term outcomes. Patients who are too unstable for immediate definitive surgery can benefit greatly from this temporary support, enhancing their suitability for more extensive interventions. The duration of IABP support varies depending on the patient’s response and the planned subsequent therapy.
IABP Complications and Management
While IABP offers significant benefits, potential complications necessitate careful monitoring and management. These include bleeding at the insertion site (femoral artery), requiring meticulous hemostasis and potential surgical repair. Limb ischemia, due to impaired blood flow below the insertion site, may necessitate adjustments to balloon inflation pressure or even removal of the device. Infection at the insertion site is another concern, demanding prompt antibiotic therapy and close observation. Aortic dissection or rupture, though rare, constitutes a life-threatening event. Careful attention to balloon inflation pressure and placement is crucial to minimize this risk. Thrombocytopenia, a decrease in platelet count, can occur, potentially increasing the risk of bleeding. Regular blood tests and appropriate management are essential. Prompt recognition and appropriate treatment of these complications are paramount to improve patient outcomes and reduce mortality.
IABP⁚ Nursing Care and Patient Monitoring
Continuous monitoring of hemodynamic parameters, including blood pressure, heart rate, and urine output, is crucial. Careful observation for signs of complications, such as bleeding or limb ischemia, is also essential. Patient education and discharge planning are integral parts of comprehensive nursing care.
Monitoring Hemodynamic Parameters
Continuous monitoring of hemodynamic parameters is critical during IABP therapy. This includes vigilant observation of arterial blood pressure, both systolic and diastolic, to assess the effectiveness of counterpulsation and identify potential complications such as hypotension or hypertension. Heart rate monitoring is essential to detect arrhythmias, which can be influenced by IABP therapy or indicate underlying cardiac issues. Central venous pressure (CVP) monitoring provides insights into right-sided heart function and fluid status, vital for managing fluid balance in patients often suffering from volume overload or hypovolemia. Accurate assessment of cardiac output, using techniques such as thermodilution or echocardiography, helps evaluate the overall effectiveness of IABP support and guide adjustments to therapy. Urine output is a crucial indicator of renal perfusion, and any significant changes should prompt investigation to rule out complications such as renal ischemia, a potential side effect of IABP. Regular assessment of these parameters, combined with careful clinical observation, ensures timely detection of problems and appropriate interventions.
Managing IABP-Related Complications
Managing IABP-related complications requires prompt recognition and intervention. Aortic dissection, a life-threatening complication, necessitates immediate surgical intervention. Limb ischemia, due to catheter placement or impaired blood flow, may require adjustments to balloon inflation pressure, heparin administration, or even surgical thrombectomy. Bleeding at the insertion site needs careful assessment and management, potentially involving local pressure, suture repair, or blood product transfusion. Infection at the insertion site can be addressed with antibiotics and meticulous wound care. Balloon rupture is a rare but serious event requiring immediate IABP removal and possibly surgical repair. Neurological complications, such as stroke or transient ischemic attack (TIA), necessitate prompt neurological assessment and supportive care. Monitoring for these complications, coupled with proactive measures such as anticoagulation management and meticulous asepsis, helps minimize their occurrence and severity. Prompt intervention is key to improving patient outcomes.
Patient Education and Discharge Planning
Thorough patient education is crucial before IABP insertion. Explain the procedure’s purpose, expected duration, potential benefits, and associated risks. Discuss post-procedure expectations, including pain management strategies, mobility limitations, and dietary restrictions. Educate patients on the signs and symptoms of complications, such as bleeding, infection, or limb ischemia, emphasizing the importance of immediate medical attention. Discharge planning involves coordinating post-hospital care, including medication reconciliation, follow-up appointments with cardiologists, physical therapy, and home healthcare services. Assess the patient’s understanding and ability to manage their medications and follow post-discharge instructions. Provide written materials, including contact information for healthcare providers and support groups. Address any anxieties or concerns the patient or their family may have, ensuring a smooth transition to home, promoting successful recovery and adherence to the prescribed treatment plan.
Leave a Reply
You must be logged in to post a comment.